Translational bioethics in nursing: a conceptual review of definitions, applications and ethical implications | BMC Medical Ethics

This section presents the results from extracting the definitions from the literature retrieved and the analysis of the definitions for defining attributes, antecedents and consequences.
Step 3: identifying uses of the concept
The Oxford Learner’s Dictionary defines translation as the process of changing something into a different form [8]. The Merriam-Webster Dictionary defines bioethics as a discipline that deals with the ethical implications of biological research and applications especially in medicine [9]. TB has been defined as “the application of legal and ethical principles to research practice or to the consultation room” [10]. It encompassed the It may also be considered as an extension of research ethics that takes into consideration societal impacts of translational research and interdisciplinary collaboration from various disciplines, including social sciences, ethics, law, and public health [11]. Furthermore, it encompasses all types of reasoning and practical conclusions, such as policymaking, that shape real-life medical and environmental decisions [12, 13]. These decisions can involve anything from clinical practice to healthcare interventions decisions [12]. TB works to close the “theory-practice gap” in ethics [7, 14, 15]. This can include guiding nurses and healthcare providers in making ethically sound decisions that reflect real-world challenges. TB is concerned with interventions, changes in practice and policies [7] and has the goal of supporting change in health systems [16]. Furthermore, the translational role of bioethics helps in guiding the refinement of clinical practices in response to ethical concerns such as patient safety [17]. TB is not for ethicists only as it is concerned with translating ethical principles to support non-bioethicists, such as researchers and healthcare practitioners, in dealing with ethical dilemmas [15]. Additionally, TB provides avenue for navigating ethical implications resulting from ongoing scientific and technological developments dilemmas [18]. Nurses, as key healthcare providers, must be able to navigate this complex landscape to ensure ethical, equitable, and high-quality care for patients.
Step 4: defining attributes
Walker and Avant [6] suggest that recurring qualities of a concept help distinguish it from others. The review of literature revealed four primary defining characteristics of TB.
Bridging the theory-practice gap
This attribute involves ensuring ethical principles are applied in real-world settings. TB seeks to close the gap between academic scholarship and contemporary policy and practice [19,20,21]. According to Lanphier et al. (2022), bioethics does not make sense without attention to the real-world practices and the lived realities of healthcare [22]. TB seeks to make a tangible difference by developing practical interventions and supporting healthcare providers including nurses and in adopting bioethical principles [2, 7]. It integrates ethical principles, particularly those focused on safeguarding human participants, into the ethical framework guiding clinical practice [18]. This attribute is therefore crucial as the “theory-practice gap” is a key and foundational problem TB aims to solve.
Ethical evaluation and decision-making
This involves examining ethical principles and their implementation in translation. High-quality translational bioethics requires attention to context [23]. TB further emphasises the critical consideration of existing real-world bioethical issues [19]. Due the changing nature of healthcare affected by factors like technological advancement and globalization, examining the ethical principles and the context of the occurrence of ethical issues is crucial. TB should convey insights on ethical issues in healthcare practice to audiences outside the traditional field of bioethics [16]. In the practice of translational bioethics, ethicists identify and analyse ethical concerns and arguments, thereby contributing to more informed and reflective decision-making processes within healthcare institutions [24]. In effect, this will help identify if the translation process helped address the initial ethical challenge or resulted in new unintended ethical concerns [25]. A collaborative effort in assessing ethical concerns and providing practical solutions and evaluating the effectiveness of the ethical solution will lead to meaningful outcomes. This attribute also requires the development of institutional policies and guidelines that describe the processes in context-based evaluation and decision-making.
Interdisciplinary collaboration
Another hallmark of TB is the collaboration between different professionals. It involves cooperation between professionals from various fields such as social sciences, ethics, public health, law, and medicine [11]. Sisk et al. [25] also argue that translating ethical norms into practice requires expertise from multiple disciplines and stakeholders. It is key to addressing the broad societal implications and ensuring that ethical decisions are made from a cross-disciplinary perspective [11, 26]. Nurses must collaborate with ethics committees, legal professionals, and other healthcare experts, as emerging ethical issues are often too complex to be addressed by a single discipline alone.
Social responsibility and societal impact
This attribute is concerned with making sure the integration of ethical principles into practice makes positive societal impact. Translational bioethics takes into consideration the social implications of bioethics research [17, 27, 28]. When considering translation within practice, some normative claims can be seen as acceptable or not depending on their impact on real-world circumstances [29]. Proponents of TB argue that it takes into account the broader societal consequences that may arise from emerging scientific advancements [26, 30]. Consider the normative claim that “all patients should be informed of incidental findings in genomic research.” While this may seem ethically sound in theory (respecting autonomy), its translation into practice may overwhelm patients with uncertain information, cause unnecessary anxiety, and burden the healthcare system with follow-up requirements. In this case, Bærøe et al. [29] suggest assessing whether this norm, when applied, promotes ethically desirable outcomes overall (in relation to beneficence and justice) rather than strictly adhering to it in all contexts.
These attributes clearly illustrate the necessary activities that must take place for TB to be fully actualized. Embedded in TB are several bioethical activities including policy development, ethical consultation, research, and public engagement.
Step 5: developing a model case
The model or sample case is a practical example of the concept under study and must contain all of the defining attributes [6]. The fictional model case below demonstrates the defining attributes of translational bioethics.
At a regional hospital, a team of gynecological oncologists and nurses noticed that most cervical cancer patients were presenting at late stages, resulting in high mortality. Data from the hospital revealed that fewer than 5% of women had undergone prior screening. Recognizing this as a serious health equity issue, the team initiated a collaborative effort involving a bioethicist, a public health expert, and community health workers. Together, they reviewed evidence on structural and cultural barriers to screening and critically assessed the hospital’s outreach, education, and service delivery practices. Their ethical analysis, grounded in justice and beneficence, highlighted systemic gaps that disproportionately affected low-income and rural women.
The team co-developed a culturally appropriate intervention that included mobile screening units, multilingual health education, and community engagement through local women’s groups. Hospital administrators supported policy revisions to integrate the program into routine services. The intervention was launched with ongoing evaluation of clinical outcomes and ethical impact. Feedback loops with community members allowed the team to adjust the approach in real time to ensure relevance, fairness, and sustainability.
Step 6: developing additional cases
Step six of Walker and Avant’s concept analysis involves a definition of other items, which may include borderline, related, contrary, or invented items [6]. A fictional borderline case, related case and one contrary case are discussed here.
A borderline case
They may contain most or even all of the defining characteristics but differ substantially in one of them [6].
Nurses in a hospital’s intensive care unit (ICU) become concerned about the ethical challenges arising from the use of life-sustaining treatments for patients with very poor prognoses. They initiate discussions among themselves and consult the hospital’s ethics committee. The ethics committee reviews relevant ethical guidelines and legal precedents to develop recommendations for improving communication with families and facilitating shared decision-making about end-of-life care. They implement training sessions for ICU staff on these recommendations.
While this initiative focuses on ethical evaluation and aims to improve practice, it lacks a significant engagement with broader interdisciplinary collaboration beyond the existing hospital structure. The impact of the training on actual changes in practice is not systematically evaluated.
A related case
Related cases are instances of concepts that are related to the concept being studied but that do not contain all the defining attributes [6].
A group of nurses in a medical department setting is conducting a study on the effectiveness of a new pain management protocol for postoperative patients. They adhere strictly to the ethical guidelines for research involving human subjects, ensuring informed consent and minimizing risks. They collaborate with nurses at surgical departments and statisticians on the research design and data analysis.
The primary focus of this research is on generating research evidence and adhering to research ethics rather than the broader, active translation of existing ethical concepts into widespread changes in healthcare policy or addressing societal implications beyond the immediate research participants.
A contrary case
Contrary cases are clear examples of “not the concept” [6]. This is a fictional contrary case.
A nurse routinely administers medications to patients without verifying patient identity or allergies, citing being too busy due to understaffing. When questioned by a colleague about the potential risks, the nurse dismisses their concerns and continues the practice. This situation demonstrates a failure to apply basic ethical principles of non-maleficence and fidelity to professional standards. There is no attempt to bridge any gap between ethical theory and practice; instead, there is a disregard for established ethical guidelines.
There is no ethical evaluation, decision-making process, interdisciplinary collaboration, or consideration of social responsibility or societal impact involved.
Step 7: identifying antecedents and consequences
Antecedents
This step helps in identifying the events or occurrences that must have occurred or existed before a concept happens [6]. The literature review revealed significant antecedents to translational bioethics.
-
1.
Recognizing the Complexity of Issues: A core precedent to TB is the identification of the complexity of ethical issues. For translation to be completed, it is essential to identify the ethical challenge [12, 25]. Nurses encounter several ethical issues in their duties which include issues surrounding end-of-life decision-making, informed consent, confidentiality and rationing of limited resources. A nurse identifies these ethical issues through comprehensive assessments of individuals, families and communities.
-
2.
Identifying a Theory-Practice Gap: Acknowledging that a gap exists motivates the need for translational bioethics to bridge it by translating ethical theories into actionable policies and practices [7]. For TB to take an effect, healthcare providers must acknowledge the need to translate ethics into practice. Nurses through comprehensive assessments of clients and communities may identify ethical concerns such as health inequalities and cultural insensitivity in care delivery. The attributes of TB can then be applied to address these concerns.
-
3.
Commitment to Real-World Impact: TB seeks to bride the theory-practice gap and hence demands a commitment to make impact. The main motivation for translational bioethics would have to be practical influence, to create change in the real world [7]. Nurses, in their daily duty execution, embody this commitment through a variety of actions that extend beyond routine clinical care.
-
4.
Shared Goals and Values: TB requires effective interdisciplinary collaboration. For this to be effective, there is the need for shared goals and values among the various participating healthcare professionals. When professionals from various fields agree on shared priorities, collaboration becomes more natural and effective [31]. In doing this, nurses play a vital role as communicators, coordinators, and advocates within the healthcare team. They contribute their unique perspective gained from close and continuous patient interaction, which allows them to highlight ethical concerns that may not be visible to other professionals.
-
5.
Institutional and Policy Support: Institutions and policies that encourage interdisciplinary collaboration provide essential antecedents. For example, academic institutions and research centers may establish interdisciplinary research teams or create joint programs that foster collaboration across disciplines [31].
-
6.
Availability of Ethical Tools and Guidelines: These tools provide the necessary resources for professionals to make ethical decisions in complex situations [2, 24]. Translational activities require self-reflexivity and ethical justification [29]. The availability of these resources is a prerequisite for effectively navigating these challenges. Structured ethical frameworks, institutional policies supporting ethical deliberation (such as ethics committees or decision-making protocols), and ethical case discussions are key strategies that guide teams through complex scenarios and facilitate collaborative ethical decision-making [32].
Consequences
Walker and Avant [6] described consequences as the events or incidents that occur as a result of the occurrence of the concept. The outcomes of TB are diverse.
-
1.
Improved Patient Outcomes: By translating ethical principles into practice, TB leads to better patient outcomes. A model application of TB resulted in mortality reduction in patients with acute ST Elevated Myocardial Infarction [1]. With such an end-goal in sight, nurses can effectively contribute to TB by integrating ethical reasoning into everyday care decisions. Through that, nurses play a pivotal role in transforming ethical principles into measurable improvements in patient health and well-being.
-
2.
Enhanced Health Equity: The goal of TB is to address fundamental societal issues, including the effects of translational science on public health, health equity, and human flourishing [31]. Majumder et al. [30] illustrated enhanced equitable access to quality care in SCD when viewed under the lens of translational bioethics.
-
3.
Increased Trust in Healthcare Systems: TB has a core principle of making positive social impact. When that is achieved, the trust in healthcare systems increases. Evans [27] demonstrated how using the concept might lead to support for research on human brain organoids. Translational bioethics can therefore increase public trust in healthcare systems and bioethical decision-making processes.
-
4.
Informed Policy and Decision-Making: TB helps policymakers by providing evidence-based ethical guidelines that shape healthcare policies and practices [7, 13, 16, 25]. Case studies of TB serve as reference points for decision makers.
-
5.
Positive Social Impact: By integrating public values and addressing the societal implications, translational bioethics can lead to positive social changes. Boyle et al. [33] based on ethical principles of beneficence, nonmaleficence, autonomy, and justice to develop a significant protocol for a labor and delivery unit during the early phase of the COVID-19 pandemic. This study resulted in the development of significant protocols in a real-world crisis [33].
-
6.
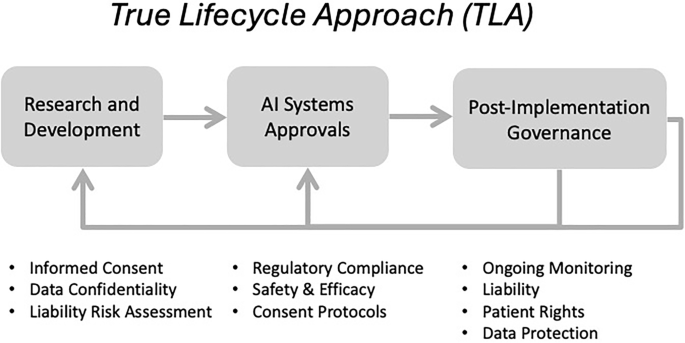
Reduction of Ethical Conflicts: Translational bioethics helps minimize conflicts in clinical settings by providing clear ethical frameworks for decision-making. It helps in resolving with cases with ethical dilemma [34]. The attributes of TB such as interdisciplinary collaboration and ethical evaluation ensure all ethical issues are resolved in the application of TB. Figure 2 presents a conceptual model of the antecedents, attributes, and consequences of TB.

Conceptual model of antecedents, attributes, and consequences of translational bioethics
Step 8: empirical referents
This involves the verification of the occurrence of the concept of TB. They are categories of actual phenomena that by their existence or presence demonstrate the occurrence of the concept itself [6].
-
1.
Development and Implementation of Ethical Guidelines: When TB is implemented successfully, there will be clear evidence of the application of ethical guidelines. Many hospitals and institutions have ethical committees that ensure ethical practice and this further ascertains a way through which TB happen. Studies that have applied TB have demonstrated this empirical referent [1, 27, 30, 33]. Crico et al. [35] found that healthcare workers including physicians and nurses perceive clinical ethic committees as helpful and valuable in improving the quality of care.
-
2.
Client satisfaction – TB occurrence can be examined through the lens of patient satisfaction. Evaluating user satisfaction helps healthcare workers in assessing the practical impact of bioethical interventions on healthcare delivery. The SERVQUAL (service quality) instrument has been a preferred tool in many satisfaction studies [36]. Nurses can conduct patient satisfaction surveys after implementing TB to evaluate its effectiveness.
-
3.
Case Studies Illustrating Ethical Decision-Making: Practical application of TB can be found in case studies, which represent concrete examples of how ethical principles are translated into real-life healthcare decisions and outcomes. TB has been documented in management of ST elevated myocardial infarction [1] and advanced cervical cancer [34].
-
4.
Policy Reforms Influenced by Bioethical Research: Legislative or institutional policy changes that result from bioethical studies serve as empirical referents. Mertz et al. [37] found 17 applications of bioethical research which included support for policy making, making recommendations on how to address ethical challenges, and pleading for stricter application of existing rules.
link